Pinnacle features among the first areas to roll out localities approach
The development of localities is set to be a fundamental part of New Zealand’s reformed health system.
Today Health Minister Andrew Little announced the first nine areas to roll out the locality approach to improving people's health.
We’re excited to share that Tūwharetoa (Taupō-Tūrangi) and Hauraki are among the first communities to be selected. This means the learnings and impacts from this new approach will be strongly experienced within the Pinnacle network.
The locality approach will replace the way things are currently done through district health boards and primary healthcare organisations. It is important to note the people doing this work now will still be involved, but we’ll be working differently.
Where are the first localities? And why?
The positive progress happening in these communities already was a big factor in their selection.
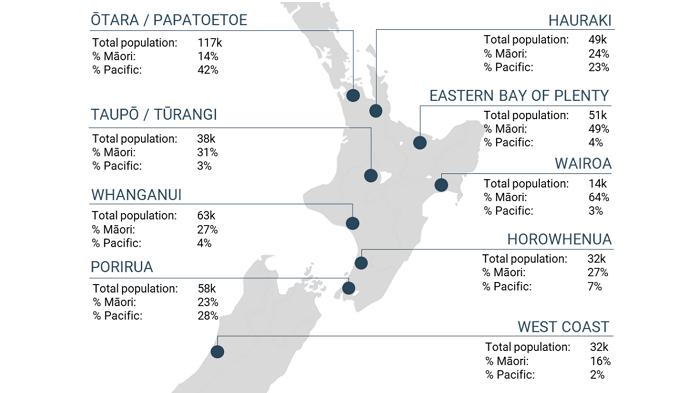
- Ōtara/Papatoetoe
- Hauraki
- Tūwharetoa (Taupō-Tūrangi)
- Wairoa
- Whanganui
- Porirua
- West Coast
- Eastern Bay of Plenty
- Horowhenua
As shown on the map above, there is emphasis on areas with a strong Māori or Pacific population along with a strong focus on rural populations. These are populations where currently services can struggle to deliver on an equitable basis.
Localities explained – in brief
A locality is essentially a place-based approach to improving the health of populations, as well as a mechanism for organising health AND social services to meet the needs identified by whānau, community and mana whenua.
There are three characteristics to a locality.
- It is a partnership with mana whenua, recognising their tino rangatiratanga.
- The approach supports locally led solutions that take a holistic approach to wellbeing, acknowledging the range of other factors that impact on a person’s health.
- The locality approach will join up care across communities and improve integration with different layers of the health system.
Localities are geographic areas that make sense to the people that live there.
- The exact geographic size, or population it serves, will change across the country, and will be determined through engagement with the community.
- The boundary lines may follow existing boundaries defined by local government or mana whenua; it will simply depend on what works best for each area.
Once the boundary is determined, people and organisations with influence over community health and wellbeing will collaborate on what outcomes they want to see for their community. This will include Iwi-Māori Partnership Boards, and ideally will include health and social care agencies and community organisations, and local government.
A three-year locality plan will be developed in collaboration with the locality partnership, Iwi Māori Partnership Boards, Health New Zealand, and the Māori Health Authority. These locality plans will detail how the goals set for a locality will be achieved.
The plans will drive procurement of services by Health New Zealand and the Māori Health Authority and be the basis for monitoring progress.
Communities and consumers of health services in the locality will be actively involved in identifying priorities and aspirations for services and outcomes.
What we can expect to see next
Where there are localities
The first localities will be stood up over April and May 2022 to provide a platform for working through the detail of how the locality approach will operate in practice.
Where localities are being rolled out, they will start to work in different ways and in collaboration with community and social care organisations.
We will see a change in traditional provider roles and service models over time, and the commissioning and development of new roles and services to meet community need. This will have impacts on general practice, and we'll be regularly updating you from what we are learning from our work with Tūwharetoa (Taupō-Tūrangi) and Hauraki localities.
The insights gained from the first localities will also help determine the support arrangements for provider networks.
Where localities are yet to be formed
The roll out of localities will happen over the next two years. New localities are expected to be stood up each quarter so that every area in New Zealand has its own locality by July 2024.
On 1 June 2022, and in areas where localities are yet to be rolled out, primary health organisations will continue to operate through existing arrangements until the new locality approach rolls out.
Pinnacle will be helping general practices in areas not part of initial localities to understand and prepare for the changes that will come.
More information on the Tūwharetoa (Taupō-Tūrangi) locality
This locality will follow the tribal boundary of Ngāti Tūwharetoa as mana whenua of this rohe.
This locality aspires to the ‘holy grail’ of health and social care integration, which includes comprehensive primary and community care teams, and will build on existing intersectoral partnerships to co-ordinate services for whānau with complex needs.
Provider networks, comprised of comprehensive community care teams, will work together to plan and deliver care and develop new community models of service delivery. Implicit to their success will be the ability to share clinical data.
The good news is we aren’t starting from scratch and there is considerable collaboration underway that we can leverage - we’ve got COVID-19 to thank for that!
Here are some Q+As that we're sure you are interested in - if you have more please contact Katie Latimer, General Manager, Strategic Development.
A locality on its own won’t solve the pervasive workforce challenges that exist for the health workforce.
However, what will make a difference is workforce optimisation, substitution, and development to ensure sustainability. We already have a range of ideas which were suggested by community health providers and know there will be more ideas we haven’t captured yet.
We will start with building on the hapū-aligned kaiāwhina workforce to reduce wait times for access to care, increase early engagement and intervention with whānau Māori, support workforce retention and build wealth in the locality. Once in place, we can look at a range of other ways in which non-GP workforces can link with general practice and support whānau.
It’s generally accepted that traditional 15-minute appointments don’t meet the needs of people with high and complex needs.
The onus is on health AND wellbeing services to determine how they support and improve equitable access for people who have traditionally been seen as disengaged from primary care, not the other way round!
Through our locality work, we will have the opportunity to re-imagine how general practice consultations are currently delivered and facilitate connections for whānau with comprehensive primary and community care teams.
A capitation review was commissioned by the Transition Unit to explore general practice sustainability and equitable funding across the health system. While the results of this analysis aren’t yet available, we hope that the existing funding formula for general practice is addressed, thereby ensuring that general practice can offer a range of services to meet individual and whānau needs.
Whānau centred care and support is also offered successfully beyond the four walls of general practice, and we will build on the work already done as part of the COVID response across the Tūwharetoa rohe to support whānau self-management and self-determination.
We are fortunate to have exceptional general practice and primary care capability across the locality.
Mature community relationships, a track record of innovation in primary care and strong leadership set us up well to think differently about the challenges primary care faces and how it can be part of the solution.
There will be regular opportunities for you to contribute your ideas and thinking, so please contact Pen Blackmore (Network Lead) or Natalie Clark (GP Liaison).
What we know:
- primary care may be asked to do more, and/or do it differently
- the PHO Agreement will be replaced in the future, but further detail is yet to be announced
- a capitation review was commissioned by the Transition Unit to explore general practice sustainability and equitable funding across the health system.
What we don't know:
- the outcomes of the capitation review – so it’s impossible to know if there will be appropriate funding to support the changes, but every indication is that it’s well understood that primary and community services have been historically underfunded and undervalued, so we are hopeful this will be recognised through further investment
- we don’t yet have full visibility of Regional Health New Zealand and/or Regional Māori Health Authority and their commissioning functions, so we don’t know how or with whom additional funding will be negotiated.
Telehealth and digital enablement have been identified as critical to the development of the locality approach, both nationally and locally.
We will leverage the existing Pokapū o Taiwhenua Network to provide more people with the care they need in their homes and communities, and establish data sharing and interoperability between providers, and develop additional digital models of care. We will also look at how we can equip our community/hapū health workforce with diagnostic equipment that can be used for telehealth assessment and treatments.
There are significant legislative, privacy and sovereignty considerations to navigate.
Health governance of a locality will look different for different localities, and it’s likely that governance will evolve over time as we understand the full extent of the reforms.
Iwi-Māori Partnership Boards also have a critical role to play, as do Health New Zealand and the Māori Health Authority as co-commissioners.
We are currently exploring a range of governance options for our locality. Ngāti Tūwharetoa will lead the development of the locality, with primary care, hospital services and community services supporting iwi aspirations.
Until the final structures of HNZ and MHA are announced it’s too early to understand the full extent of our connection with these functions.
More information on the Hauraki locality
The development of this locality is being led by:
- Te Korowai Hauora o Hauraki, Kaupapa Māori PHO
- Waikato DHB
- Hauraki Maori Trust Board (Mana Whenua)
- Marae Tukere (Mana Whenua)
Pinnacle, Hauraki PHO and National Hauora Coalition will work together in the roll out. We'll bring your more information as we can.
Official announcements
- First areas to roll out localities approach confirmed - News announcement, Future of Health website
- Localities update for the health sector, April 2022 on the Future of Health website. This is a seven page document that covers a range of questions you will have on localities.
- Localities information - How our health system is changing, Future of Health website
- Minister's announcement and speech
For more information
Katie Latimer, General Manager - Strategic Development
Katie.Latimer@pinnacle.health.nz
During the COVID-19 lockdown virtual consultations for POAC cases were funded. We are pleased to announce that this will be a permanent change.
Read moreFunding is now available for primary care, community, and rural health providers who are committed to supporting graduate registered nurses (RN) as they transition into practice. To be eligible for placement funding, employers must employ a graduate RN, provide preceptorship and clinical support, and hire the graduate RN for a minimum of 0.6 FTE for a period of 12 months or more.
Read moreThe extended care team is available to compliment the care you provide to your patients.
Business rules for the Primary Options Acute Care programme (Lakes), which supports primary care through funding specific clinical services.