Wellbeing - support services for patients
Support services for patients facing mental and physical wellbeing challenges are changing.
Current referral based primary mental health services are not keeping up with the demand. These services are not meeting the needs of many high needs groups – particularly Māori.
Pinnacle has been working collaboratively at a national level for some time to re-imagine the primary care response for patients facing mental wellbeing challenges.
In response to He Ara Oranga, the Report of the Government Inquiry into Mental Health and Addiction, the Wellbeing Budget 2019 provided an investment to increase access to, and choice, of primary mental health and addiction services as a critical first step in transforming mental health and addiction services in Aotearoa.
Pinnacle services
- Te Tumu Waiora in Lakes
- Te Manawanui in Taranaki
Integrated primary mental health and addiction services - a new model
This new model is about accessible, engaging, connected care.
The integrated primary mental health and addiction service makes a range of supports rapidly available to a general practice’s enrolled population to help people manage challenges that adversely affect their wellbeing.
The integrated model is about mental and physical health concerns – including thoughts feelings or actions that are impacting on health and wellbeing – so when people are in distress, they know there is appropriate support available that is easily accessible. Health and behaviour are so intertwined that it can be difficult to find any medical problem that does not involve behaviour in some way.
The types of support available for people experiencing distress includes self-management support, brief interventions, and social and cultural supports.
The government intent is to expand access to the services around New Zealand over a five-year period (roll out commenced in June 2019).
The integrated model is a national model but allows for local ‘flavour’ – it provides a framework for integrating mental health providers into primary care settings. It changes how mental health providers practice in that setting, how general practices work, and how they integrate for the health of the population.
The known benefits of this service to patients and whānau include:
- easier access to services
- a person-centred approach that understands a person’s broader life context rather than a clinical or diagnosis led model
- easier for people to talk and share how they’re feeling and giving practical support that is easy to follow through on
- peace of mind for GPs and the general practice team knowing that people can speak with someone that day, rather than being placed into an impersonal referral process.
New model, new roles
The new model of care is simple.
Health improvement practitioner
A health improvement practitioner (kaiw’akaako-a-’auora in Taranaki) -often referred to as a HIP - is a person with health experience/qualifications. The HIP role is embedded within a group of general practices. They form relationships with the members of the practice and are available to meet with people who are connected with the practice to listen, understand and provide advice. They provide brief evidence-based behavioural interventions to individuals, groups and whānau for both mental health and physical health conditions in people of all ages. When appropriate, they introduce the kaitautoko to provide health coaching and self-management support to the client.
Health coach/cultural support worker/community support worker
A health coach/cultural support worker/community support worker (kaitautoko in Taranaki) with relevant lived experience, relationships and connections walks alongside whānau to support and navigate them as they seek to achieve their health and wellness goals. They are closely connected with one or more health improvement practitioner, working in partnership to support whānau throughout the regions.
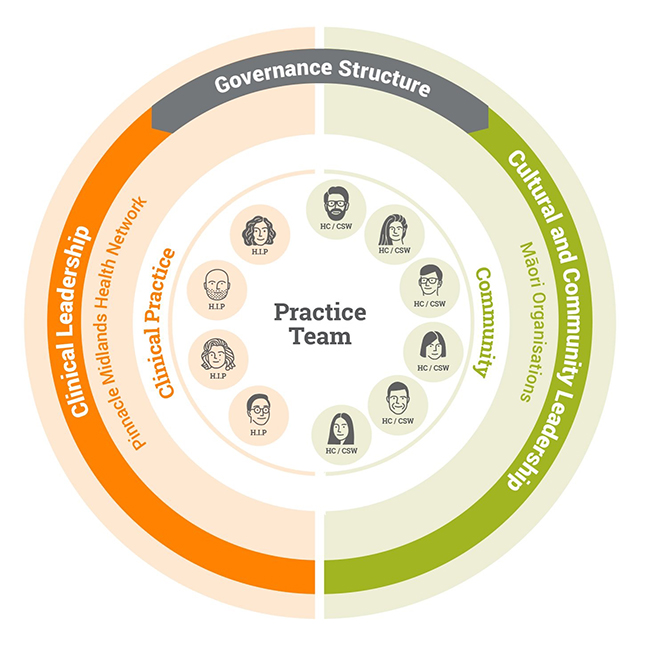
Working as an integrated team
The health improvement practitioners and coaches/support workers from across the region form an integrated team that shares learning, insight and best practice.
The collective of employing and supporting organisations provide wrap around support and leadership related to clinical practice, cultural capability and community connectedness and relationships.
Both these practice team members support patients, but also support up-skilling of existing GPs, and practice nurses to ensure they are confident and capable.
Both roles:
- see high volumes of patients (approximately 10 patients per day)
- provide a rapid response (targeting same day delivery of interventions)
- have proven outcomes
- are part of a national programme with ongoing training support and supervision.
Support is provided in a different way
Health improvement practitioners have both scheduled and unscheduled appointments.
Unscheduled patients are identified using a ‘warm handover’ from a member of the general practice team (e.g. at a time of distress).
Scheduled appointments are follow-up appointments, next day bookings or targeted patient groups.
Anyone in the practice team can initiate contact with the the HIP or health coach.
The Te Tumu Waiora integrated mental health and wellbeing service has been up and running in general practices in Taupō and Tūrangi since July 2019. The response from practices and the community has been overwhelmingly positive.
Read moreThis is a one-off grant is for primary care nurses working in general practitioner and nurse practitioner practices, schools and other primary care settings to build their knowledge and skills in mental health and addiction.
Read moreThis service is designed to support a co-response team where mental health clinicians, kaimahi Māori, Police and St John will work together when responding to mental health emergency calls.
View detailsIn addition to Pinnacle MHN primary mental health services, here are some other alternatives that may be available.